The Virus Crisis Is Underestimated
Open letter to the Minister of Public Health.
February 27, 2020
Madam Minister,
Your public statements suggest that you do not fully understand the nature of the danger that Belgium and the rest of the world face. Naturally, you trust your group of experts who are unanimous in their view that Belgium is ready to face this new coronavirus.
I sent you a file via the SPF Health website on February 12, which indicates that if the proportion of symptomatic cases due to the new coronavirus reaches 1% of the population, we would be on the verge of a hospital crisis (your reference: CCAL0331485).
In an interview published yesterday, you answer the question But how many beds do we have exactly? You know that in Belgium we have enough beds and sufficient treatment capacity. It’s an advantage. When we compare with a winter flu and the number of elderly patients who are generally hospitalized, the situation is identical.
In my file, I cited a W.H.O. February 10 report estimating that ~ 16% of symptomatic patients were in a condition serious enough to require hospitalization. For the flu it is only ~ 0.2%! The relationship between the two? A factor of 80, not really an identical situation.
The fact-finding mission of the W.H.O. in China released its report yesterday, it is worth consulting. We now have more precise figures for symptomatic patients: 80% of mild cases (can stay at home), 13% of severe cases (hospitalization), 6% of critical cases (intensive care).
Would you be so kind, Madam Minister, you who have access to all the information on the Belgian hospital network, to calculate for our edification: how many symptomatic cases would it take for the Belgian hospital system to run out of hospital beds for severe and critical cases?
There is a cacophony of incorrect information circulating not only in the print and audio-visual media about the new coronavirus, but also on the SPF Health and Sciensano websites. The official position appears to be that COVID-19 is a SARS-2.0 and therefore the measures that would be appropriate for SRAS-1.0 will be suitable for COVID-19.
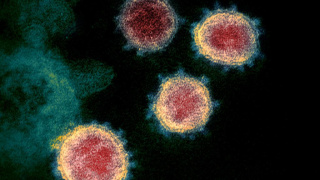
This is unfortunately a false equivalence and it is urgent to understand the essential difference between the spread of the virus responsible for SARS-1.0 and that of the new coronavirus. SARS-CoV was mainly transmitted by surface contamination and by small droplets, which travel no more than one meter, but rarely by aerosol. Everything indicates that a significant proportion of transmission of the new coronavirus is by aerosol, which completely changes the situation for isolation measures.
The first cases of SARS in November 2002 were detected in the city of Shenzhen, 7 million people at the time, and ultimately infected 5,327 people in China. The first cases of COVID-19 were detected in December 2019 in the city of Wuhan, 11 million inhabitants, and has infected 78,497 individuals in China to date (according to the Chinese government; nearly one million according to some epidemiologists), the first indication of the difference between the two viruses.
The basic reproduction number of the new coronavirus is between 4.7 and 7 according to the calculations of different epidemiologists, which is different from the actual reproduction number calculated by the O.M.S. (2,5), the difference being that the basic number corresponds to the situation without isolation measures, and the effective number changes according to the implementation of different isolation measures.
Take the situation of Italy. The first two cases were confirmed in Milan on January 31 and we are 27 days later at 528 cases. Epidemiology tells us to take the logarithm to base 2 of 528 cases divided by the two initial cases, namely approximately 8, and therefore the number of cases doubled every 3.3 days, close to doubling every 2.4 days in the absence of isolation, and while isolation measures have been in place for a few days. These figures are consistent with a high basic reproduction number.
So, we have an epidemic at least 10 times larger than SARS-1.0 at the same time in China, a new coronavirus of great intrinsic contagiousness, epidemiologists who calculate that one infection in two could be caused by a person still asymptomatic, and we also have multiple episodes of super contagion. What to conclude? You won’t find many transmission experts who will tell you anything but this new virus is spread by aerosol.
You recognize that the virus is more contagious, but what is the full implication? If the flu virus infects 2 to 8% of the population, year after year, and this virus is more contagious than the flu, what will prevent it from spreading at least like the flu in an immunologically naive population? And this is where the question of availability of hospital beds takes on its full significance and urgency, given the much higher rate of complications with this coronavirus.
It is not necessary to have a debate among the experts, although in a crisis situation it is always good to confront the divergent views of the experts. Indeed, the Public Health function it to prepare for the worst scenario, not the most rosy. Experts and officials in other western countries also recognize the seriousness of the risk we all face.
You told us that the objective is “to keep the virus out of the country as long as possible thanks to adequate surveillance of the territory“, but we learn from a courageous nurse who returns from Veneto, a region of Italy with a few cases of COVID-19, that not only are we not asking them to isolate themselves, and we are asking them to return immediately to work, but in addition we refuse to test them!
Not only is she not tested, but she also tells us that there is actually an omerta against screening for the new coronavirus for cases of flu symptoms not related to a Chinese connection. Explain to us, Madam Minister, exactly how you adequately monitor the territory when the most basic screening is not done?
If you know of a more effective, more adequate means than systematic screening to monitor the territory and keep the reproduction of this virus to a minimum in our country, please do not wait any longer to share it with us.
General practitioners are concerned about the lack of serious communication from the Ministry of Health, an email is not enough in this situation. They contrast the current response to that during the H1N1 epidemic in 2009 when they received clear information and masks. Nor should we ignore their request to have a system in place to support individuals who should remain isolated.
It is true that there was at least one vaccine in the case of H1N1, but if I am not mistaken, would not the absence of a vaccine in this case not be a reason for taking this coronavirus epidemic more seriously?
Why wait to protect medical personnel? Would we be so short of the necessary equipment? What is the situation from a logistical point of view? You say we are ready, but we would not even have masks for general practitioners?
What would you say to the families of infected or even deceased medical personnel, if we were to deplore victims whose infection could have been prevented by the earlier implementation of personal protective measures?
Zhong Nanshan, who heads the COVID-19 team of experts at the Chinese Ministry of Health, said the epidemic had been “a hard lesson” for the country: “If we had taken strict prevention measures in early December or even early January, it would have greatly reduced the number of sick, ” he said at a press conference.
The Chinese authorities made the same initial error with SARS and COVID-19, but have since mobilized to fight the virus with the extremely strict measures that are necessary when a virus is transmitted by aerosol and asymptomatically. We are making the same initial mistake as the Chinese!
And lessons must be learned now from the first phase of this epidemic, how the Chinese have moved from a very large quarantine model, 400 million people, to a flexible and targeted approach. The number of cases that will emerge as the population returns to normal remains to be seen, but the very advanced surveillance system suggests that they will be able to contain these new cases.
Shouldn’t we follow the lessons of China, and also follow the adage that prevention is better than a cure? It is imperative to mobilize the population and all healthcare personnel to allow prevention to play its role.
Fear is an essential emotion for our survival. Fear can be rational, like fear can be irrational, but your optimism is difficult to justify, Madam Minister, it is irrational.
I want to cross my fingers with you that Belgium will be spared and that the spread of the virus will slow down with the end of winter, but I cannot accept that you cross your arms in your role as Minister of Public Health .
For an effective intervention, we are in stoppage time, Madam Minister, we must no longer procrastinate.